Microbes

E Coli
Escherichia Coli is a common microbe in the environment and with humans. It is normally benign, even protective as a member of healthy gut flora. E. Coli, however, is very adaptive at becoming antibiotic resistant and represents a major health concern.
Infection with Shiga toxin-producing E. Coli (STEC) can lead to a serious health condition called hemolytic uremic syndrome (HUS).
Diarrhoea causing E. Coli can be drug resistant via the production of extended spectrum beta lactamase, making a treating antibiotic difficult to find.
In a study by Alharbi et al, more than 50% of E. Coli isolates obtained from wound infections were resistant to cefazolin, ampicillin, cefuroxime, ciprofloxacin, mezlocillin, moxifloxacin, piperacillin, and tetracycline.
The 2022 GRAM (Global Research on Antimicrobial Resistance) Study which tracked data from 2019, recorded a total of 950,000 deaths due to E. Coli.
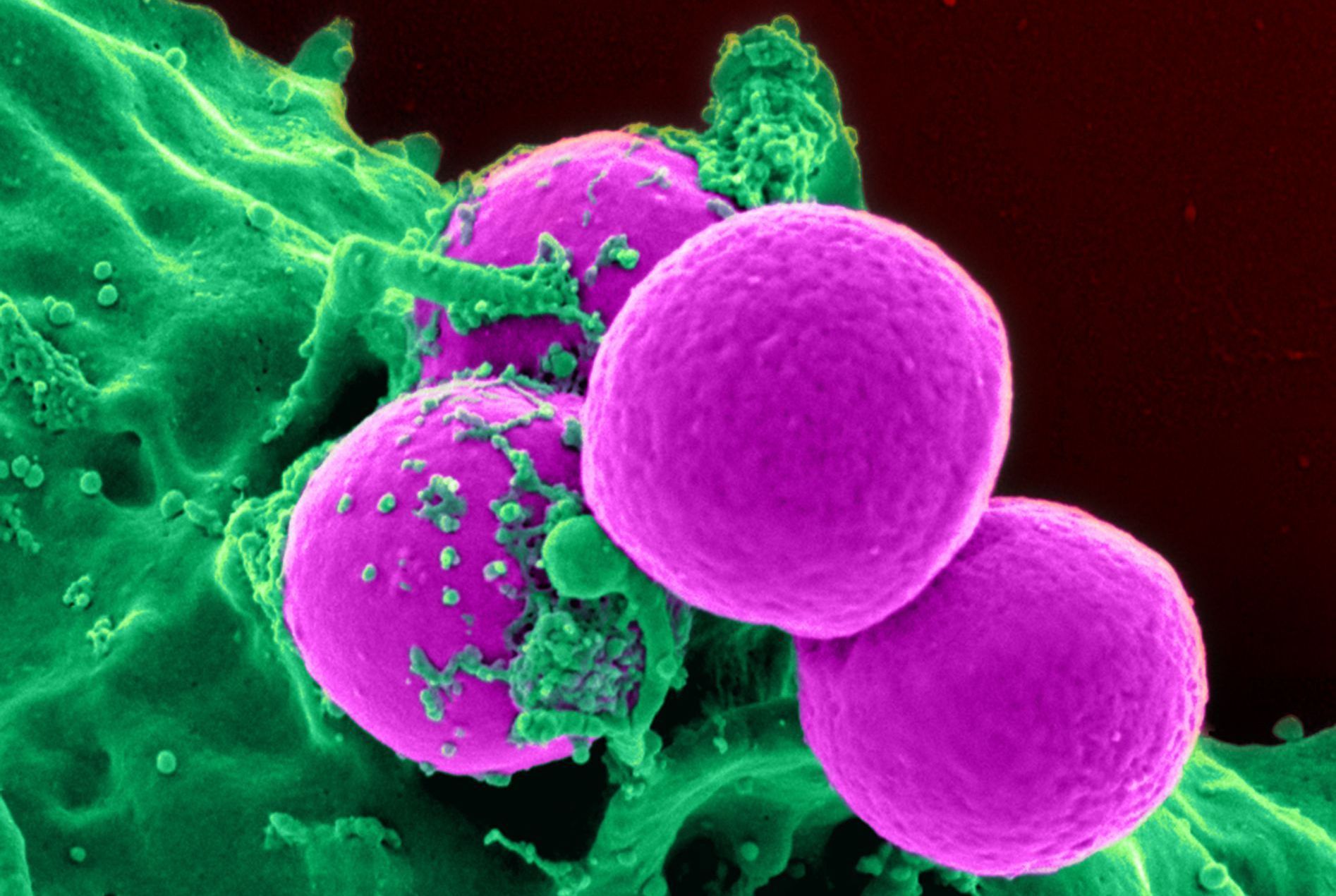
MRSA (Methicillin Resistant Staphylococcus Aureus)
MRSA is one of the leading causes of hospital acquired infections and is often associated with significant morbidity, mortality and increased hospital stay and healthcare costs.
MRSA was first described in 1961 and has increased as a health burden and threat ever since. MRSA was the deadliest pathogen-drug combination globally in 2019: the bacteria had 121,000 deaths attributed to antimicrobial resistance, according to IHME findings (Lancet, January 2022). The CDC (Center for Disease Control) lists MRSA as an urgent threat.
Resistance is conveyed through a mutation in the microbe’s penicillin binding protein.
MRSA can cause skin and soft tissue infection, bone and joint infection, pneumonia, bacteraemia and endocarditis.
MRSA is a widespread threat in hospitals and aged care (up to 16.29% in aged care facilities (Hasanpour et al, Antimicrobial Resistance and infection Control 4(2023)). Healthcare workers are carriers of MRSA, with a pooled prevalence rate of 9.23% (Giri et al (American Journal of Infection Control, Feb 2023)).

Klebsiella Pneumoniae
Klebsiella Pneumoniae is a major AMR disease burden and increasing health threat. In July 2024 WHO issued a news release describing hypervirulent strains of Klebsiella Pneumoniae which have the capacity to infect healthy as well as immunocompromised individuals and produce invasive infections which are resistant to last line antibiotics such as carbapenems.
Klebsiella Pneumoniae is associated with pyogenic (fever producing) liver abscess, and causes pneumonia, particularly in immunocompromised hospital patients. It is also unfortunately a leading pathogen in neonatal deaths.
The microbe is particularly capable of producing plasmids which can disseminate drug resistant AMR genetic material to other microbes.

Pseudomonas Aeruginosa
Pseudomonas aeruginosa is a versatile and opportunistic pathogen known for its significant antimicrobial drug resistance, which poses a serious threat in healthcare settings. This bacterium is capable of acquiring resistance to multiple antibiotics through various mechanisms, including the production of β-lactamases, efflux pump overexpression, and changes in membrane permeability. As a result, infections caused by P. aeruginosa are often difficult to treat and can lead to increased morbidity and mortality.
P. aeruginosa is associated with a range of clinical infections, including:
1. Hospital-acquired pneumonia: Particularly in ventilated patients.
2. Urinary tract infections: Common in individuals with catheterization.
3. Wound infections: Especially in burn victims or surgical patients.
4. Bloodstream infections: Often seen in immunocompromised patients.
5. Cystic fibrosis-related infections: Chronic lung infections in affected individuals.
The increasing prevalence of multidrug-resistant strains of P. aeruginosa underscores the need for ongoing surveillance, research into new antimicrobial therapies, and effective infection control measures.

Candida Albicans
Candida Albicans is a very widespread pathogenic yeast which causes dermal, oral, vaginal and systemic infections. Its resistance to antifungal agents, particularly azole antifungals represents a pressing threat to global healthcare.
Candida albicans causes > 150 million mucosal infections and ~200,000 deaths per annum due to invasive and disseminated disease in susceptible populations. Economically, yearly healthcare costs for Candida infections in the USA are ~$2 billion [2], with similar per capita costs in the European Union. C. albicans accounts for ~75% of all Candida infections and is an enormous global health burden, the severity of which continues to escalate. Jonathan Richardson, Pathogens, April 2022).
