The AMR Crisis
The Antimicrobial Resistance Crisis
Modern medicine and healthcare are founded on the efficacy of antibiotics. This efficacy of conventional antibiotics is in a state of peril due to Antimicrobial Drug Resistance (AMR). AMR is one of the world's biggest health problems, with approximately 1.27 million deaths directly due to AMR and 4.95 million deaths associated with AMR in 2019 (ref: Lancet “Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis” Jan 20, 2022) and as many as 10 million deaths per year projected by 2050 if current trends are left unchecked (according to estimates from the 2016 UN Report on Tackling Drug Resistant Infections Globally).
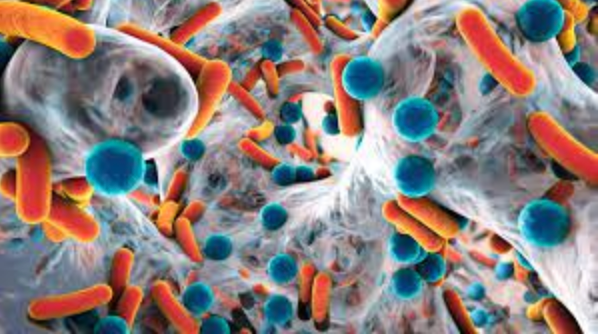
Biofilm of antibiotic resistant bacteria
In the Lancet study, six pathogen types were responsible for 73% of deaths.
These pathogens are:
Escherichia coli
Staphylococcus aureus
Klebsiella pneumoniae
Streptococcus pneumoniae
Acinetobacter baumannii
Pseudomonas aeruginosa
A major part of the microbial resistance problem is that most antibiotics comprise one type of molecule, and use one mechanism of action for their efficacy, so that microbes only need one piece of adaptation to acquire resistance.
The use of modern antibiotics and the development of microbial resistance against them may be summarised as follows:
| Antibiotic | Year of Introduction | Year Resistance Recorded | Years to Resistance |
|---|---|---|---|
| Sulphonamides | 1936 | 1942 | 6 |
| Beta Lactams, Penicillin | 1938 | 1945 | 7 |
| Aminoglycosides, Streptomycin | 1946 | 1946 | 0 |
| Chloramphenicol | 1948 | 1950 | 2 |
| Macrolides, Erythromycin | 1951 | 1955 | 4 |
| Tetracyclines, Chlortetracycline | 1952 | 1950 | -2* |
| Rifamycins, Rifampicin | 1958 | 1962 | 4 |
| Glycopeptides, Vancomycin | 1958 | 1960 | 2 |
| Quinolones, Ciprofloxacin | 1968 | 1968 | 0 |
| Streptogramins, Streptogramin B | 1998 | 1964 | -34* |
| Oxazolidinones, Linezolid | 2000 | 2001 | 1 |
| Lipopeptides, Daptomycin | 2003 | 1987 | -16* |
| Diarylquinolones, Bedaquiline | 2021 | 2006 | -6 |
Asterisk denotes that resistance identified before antibiotics official clinical launch.
(Adapted from Nature Reviews Drug Discovery ISSN)
Due to the emphasis of antibiotics being de novo, patented, expensive single molecules, often with restricted commercial availability due the emergence of drug resistant pathogenic species, their economic viability is marginal. If resistance development is sufficiently great, the commercial life of the antibiotic ends and it is added to the "antibiotic graveyard" of obsolete compounds.
For these reasons many major pharmaceutical companies have closed their antibiotic research and development programs. Primary antibiotic development then falls to smaller corporations. A report by the Biotechnology Innovation Organisation ("The State of Innovation in Antibacterial Therapeutics" Feb. 2022) estimated that 81% of new antibiotics in the current pipeline were discovered by small corporations. Because of challenges in the market, along with conventional antibiotic development costs which may exceed US $1 billion, it means that businesses may struggle even after successful regulatory approval.
